Author Name:
SEOK WOO YANG, MD & PhD
Contact information:
E.mail: soplab@outlook.kr
Date:
2020.03.10
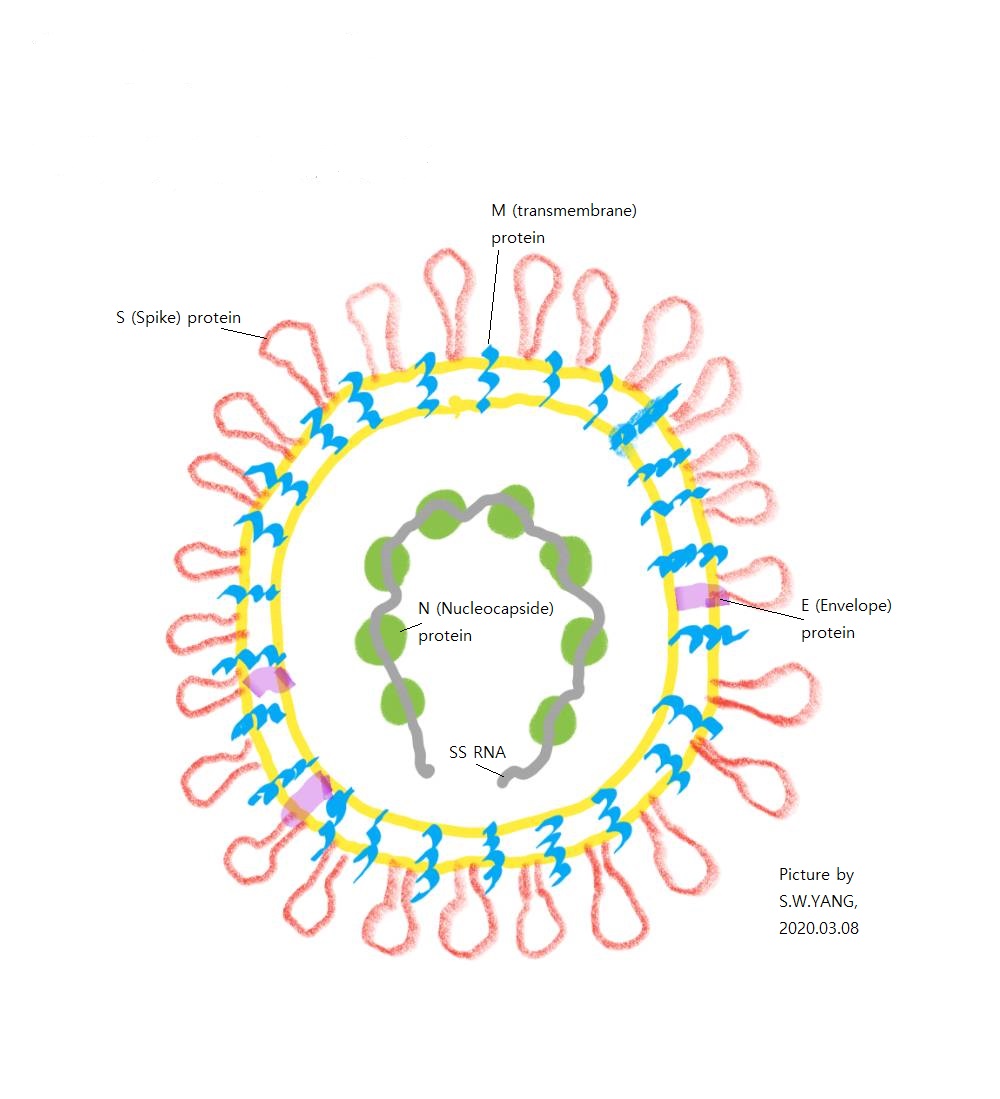
As of 9th Mar. 2020, a novel coronavirus (2019-nCoV, COVID-19) has been highly contagious and its clinical outcome is unpredictable. The main cause of death is acute respiratory distress syndrome and the next things are heart and renal failure.
About the pulmonary pathologic findings in the autopsy cases of COVID-19, Xu et al reported that diffuse alveolar damage with desquamation of pneumocytes, intra-alveolar fibromyoid exudate, and pulmonary edema, indicating acute lung injury, pathologically and acute respiratory distress syndrome(ARDS), clinically. In contrast, the tissue destruction of the heart and the liver was not remarkable like the lung. In the pulmonary lesion, there were high concentration of both Th17 cells among CD4 helper T cells and cytotoxic T cells with cytolytic granules, like perforin and granulysin. This cytolytic injury can be interpreted to have a correlation with the pulmonary pathologic findings of COVID-19. Th17 CD4 cells contribute to activation of cytotoxic T cells with cytolytic injury. Th17 CD4 cells are polarized by IL-6 and TGF-β which activate Th17 transcription factor RORγt.[1]
In this context, if IL-6 and TGF-β can be suppressed, the detrimental lung injury by T17-CD4 cell-induced cytotoxic T cells may be lessened. As the representative antibiotics for this assumption, roxithromycin and cefuroxime can be candidates. These antibiotics reduce the production of IL-6 and TGF-β.[2],[3]
About the reason why roxithromycin and cefuroxime can be feasible therapeutic antibiotics, there is a supportive molecular mechanism. The pulmonary infection by coronaviruses shares the inflammatory responses by Mycoplasma pneumoniae and LPS(lipopolysaccharide found in Gram-negative bacteria), in which IL-8 and IFN-γ react with CFTR(cystic fibrosis membrane conductance regulator) on the lung epithelium and contribute to the pulmonary infection.[4] The kinds of pulmonary infection through this inflammatory pathway are as follows:
(1) Mycoplasma pneumoniae, which is usually treated by macroride antibiotics like roxithromycin and erythromycin.
(2) LPS by Gram-negative bacteria. The Gram-negative bacterial pneumonia in association with coronaviruses are caused by Gram-negative bacteria. Cefuroxime is one of many antibiotics for Gram-negative bacteria.
Alveolar macrophages play a central role in orchestrating inflammation of ARDS.[5] Once alveolar macrophages are stimulated, one of the pulmonary inflammatory responses is to damage lower respiratory tract and alveoli, especially alveolar type 2 epithelial cells.
In summary, in terms of the above inflammatory mechanisms, the therapeutic strategy to prevent ARDS can be inferred, as follows:
(1) Steroid as inhalant or oral intake to block the inflammatory responses by alveolar macrophages.
(2) Macroride antibiotics or cefuroxime to suppress the cytokine immune reaction by T17 CD4 cell-mediated cytolytic cytotoxic T cells.
References:
1. Xu Z, Shi L, Wang Y, Zhang J, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;S2213-2600(20)30076-X.
2. Urasaki Y(1), Nori M, Iwata S, et al. Roxithromycin specifically inhibits development of collagen induced arthritis and production of proinflammatory cytokines by human T cells and macrophages. J Rheumatol. 2005; 32:1765-74.
3. Lannergård A, Viberg A, Cars O, Karlsson MO, Sandström M, Larsson A. The time course of body temperature, serum amyloid A protein, C-reactive protein and interleukin-6 in patients with bacterial infection during the initial 3 days of antibiotic therapy. Scand J Infect Dis. 2009;41:663-71.
4. Peteranderl C, Sznajder J, Herold S, Lecuona E. Inflammatory Responses Regulating Alveolar Ion Transport During Pulmonary Infections. Front Immunol, 8, 446, 2017.
5. Aggarwal NR, King LS, D'Alessio FR. Diverse macrophage populations mediate acute lung inflammation and resolution. American journal of physiology. Lung cellular and molecular physiology. 2014;306:L709–25.