AUTHOR: SEOK WOO YANG, MD & PhD.
CONTACT: Email: soplab@outlook.kr
DATE: 2020.07.22
CONTENT:
About the facial mask-wearing, there have been many debates about the efficacy to block the viral particle spread.
The author has also fully recognized the incompleteness of the facial mask to prevent the viral particle spread perfectly.
Nonetheless, the author emphasizes the facial mask-wearing, as the following reasons:
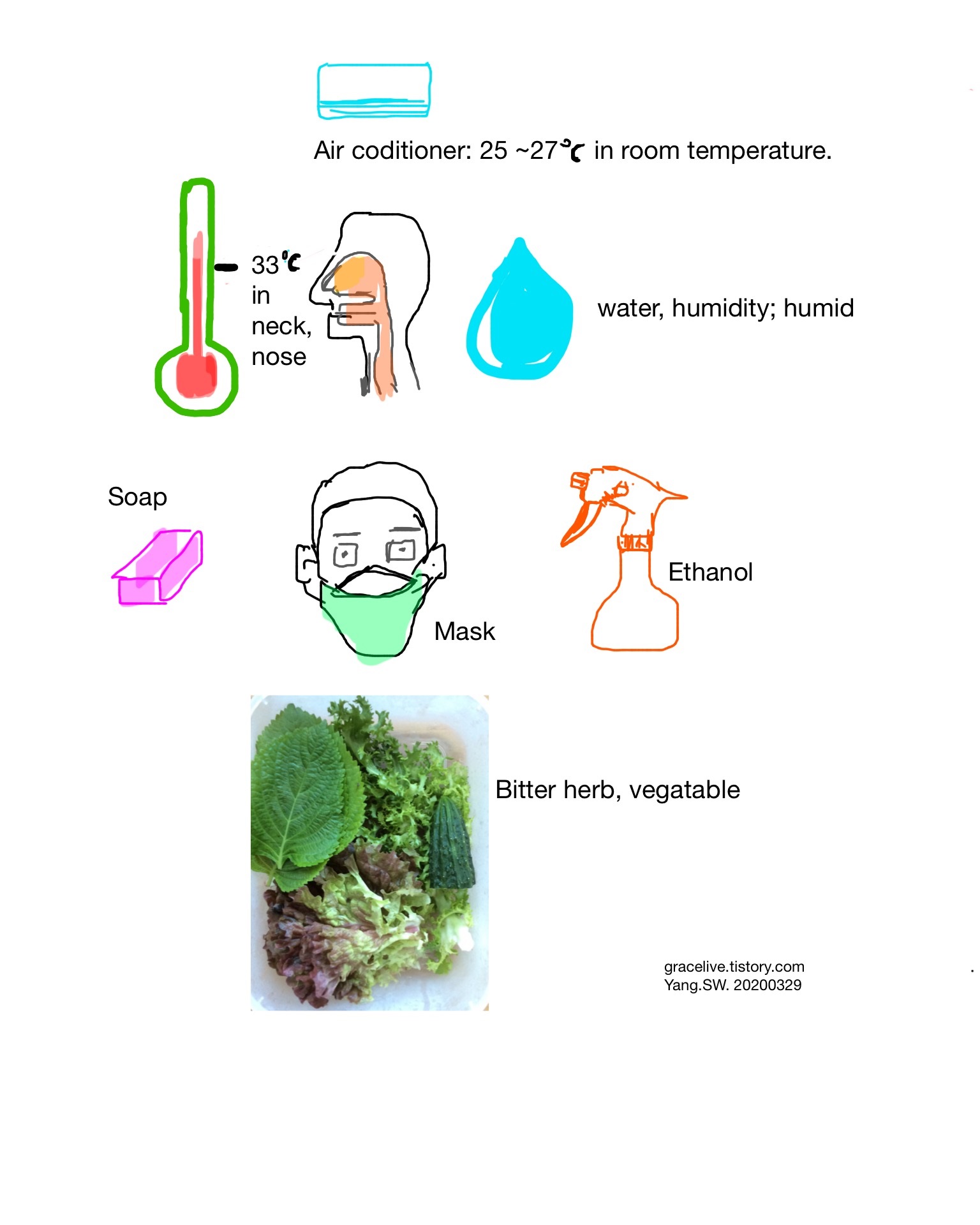
1. The known key factors to facilitate the spread of respiratory droplets including viral particles are humidity and temperature in the environmental air. The environmental air humidity and temperature vulnerable to COVID-19 is not affected by the seasonal weather, for even in summer, many people live in the air-conditioned situation. With the reasons posted in [ https://gracelive.tistory.com/39?category=838022 ], the facial mask is helpful to keep our air-way mucosa from being infected by COVID-19 and other viral disorders.
https://gracelive.tistory.com/39?category=838022
How to manage temperature & humidity to cope with Coronavirus 19?
Author: SEOK WOO YANG, MD & PhD (E.mail: soplab@outlook.kr) Date: 2020.03.04. Content: To prevent further spread and contagion of coronavirus 19, two environmental factors like temperature and hum..
gracelive.tistory.com
2. In 2008, MacIntyre et al reported that the masks as a group had protective efficacy in excess of 80% against clinical influenza-like illness. They concluded that in compliant mask users, masks were highly efficacious to prevent the respiratory viral transmission [ www.ijidonline.com/article/S1201-9712(08)01008-4/fulltext ].
This finding can be checked in the case of Taiwan and Iceland during COVID-19 pandemic, where the early facial mask and social distance were adopted and applied in two nations [ https://theconversation.com/what-coronavirus-success-of-taiwan-and-iceland-has-in-common-140455 ].
What coronavirus success of Taiwan and Iceland has in common
Taiwan and Iceland both deployed a cooperative strategy early on in the COVID-19 pandemic – and it's helped win public trust.
theconversation.com
Similarly, Singapore and HongKong showed remarkable success in the early prevention of COVID-19. South Korea (ROK), where even opened to China, became to suppress the further spread of COVID-19 as time went on. [ https://www.weforum.org/agenda/2020/04/should-we-be-promoting-the-widespread-use-of-masks/ ]
What is the evidence on wearing masks to stop COVID-19?
A doctor presents the evidence for the role of masks in containing the pandemic.
www.weforum.org
3. About above 1. & 2., the author speculates the background medical mechanism why these events happened as the mechanism of live attenuated vaccine effect. Although the facial mask is not perfect to block the viral particle spread via respiratory droplets, the amount of spread viral particles must be reduced down, to some extent. The reduced amount of viral particles can be presumed to act as the live attenuated vaccine effect rather than pathogenic(causing to provoke disease condition) effect.
Passover in the Old Testament may be a suitable historic case for live attenuated vaccine effects. The air containing certain microorganisms was penetrable to all houses of Israelites and Egyptians. The only different point is that the houses of Israelites were painted with sheep blood on the doorframes. The author infers the sheep blood on the doorframe might be functioned as a filter like a facial mask for air-borne viral or bacterial particles. The reduced amount of microorganisms might act as live attenuated vaccines rather than pathogens.
[ https://gracelive.tistory.com/53?category=838022 ]
Passover and Blood on the doorframe vs Facial Mask.
Passover and Blood on the doorframe Author: SEOK WOO YANG, M.D. & Ph.D. Contact: E.mail: soplab@outlook.kr Chapter 12 of Exodus in Bible reports on Passover day. Here God ordered the Israelite to av..
gracelive.tistory.com
Cautiously, the author predicts that the herd immunity to COVID-19 can be achieved as time goes on, like Rabies, Influenza, and other viral diseases, without an increase in mortality rate when with the above reasons.